![Revolutionizing Reproduction: How Artificial Womb Technology Solves Infertility [A Personal Story + 5 Key Stats]](https://thecrazythinkers.com/wp-content/uploads/2023/04/tamlier_unsplash_Revolutionizing-Reproduction-3A-How-Artificial-Womb-Technology-Solves-Infertility--5BA-Personal-Story--2B-5-Key-Stats-5D_1682861203.webp)
What is artificial womb technology?
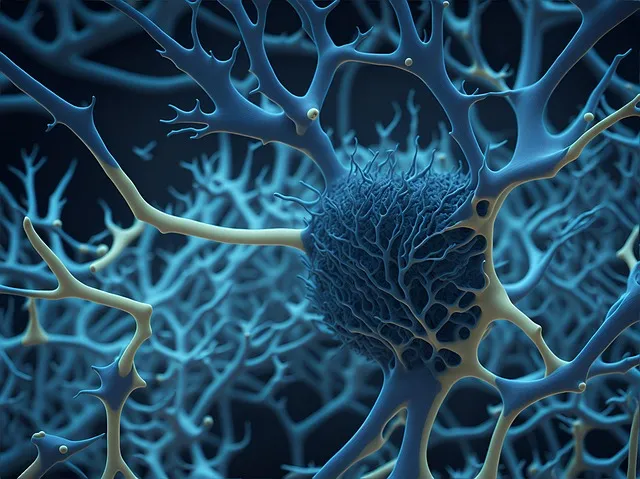
Artificial womb technology; is a method of gestating and growing embryos outside the human body inside an artificially created environment. This technology aims to create a controlled, nutrient-rich space that simulates the conditions of a natural uterus, enabling successful fetal development.
With recent advancements in biomedical engineering and neonatology, scientists have been able to recreate the necessary conditions for fetal growth such as fluid exchange, temperature control, and gas transfer. By using this technique, experts hope to reduce maternal mortality rates, save premature babies’ lives & keep them healthy by providing advanced care earlier than current medical options permit.
This breakthrough has redefined what we know about pregnancy. While still in developmental stages research continues on identifying better ways on feeding oxygen to developing fetus, improving maintenance mechanisms like umbilical cord blood sampling etc.,
Artificial Womb Technology: A Step-by-Step Guide
The concept of an artificial womb might seem like science fiction, but it’s closer to becoming a reality than you might think. The technology exists and researchers have already made significant progress in developing it further.
The idea behind an artificial womb is to provide an environment that mimics the conditions of a natural one, such as temperature, oxygen levels and other factors, allowing a fetus to develop outside the mother’s body. This could be used for premature babies born before term or for women who can’t carry pregnancy due to medical reasons.
Let’s delve into how this form of technology has evolved over time and what will hopefully come next:
Step 1: Early Attempts
Starting early on with animal models in the late 1950s by scientists at Cornell University produced little success because they couldn’t get embryos to survive longer than six days inside the machine.
Step 2: Biobag
Few decades later during mid-1990s similar experiments were carried out at Children’s Hospital Philadelphia supported by NIH grants where team led by Dr Alan Flake from CHOP developed biobags filled with amniotic fluid that worked as artificial wombs thereby extending fetal life upto extra four weeks (from lab studies). In December ‘17 human trial was successful using CCHMC/Intrexon systems inc.
Step 3: Developmental Milestone
After hours spent perfecting the design while ensuring optimal temperature regulation settings along with computer controlled blood flow – Italy lead research published their findings in renowned journal which detailed lambs surviving full development in utero synthetic environments when monitored clinically After birth immune system was studied — no differences among animals raised normally signifying lack impact modern machinery related challenges within biological processes.
Step 4: Roadmap Ahead
Although promising results are received yet numerous challenges remain viable for practical implementation involving ethical issues around removing mothers from gestational process thus lessening emotional connection between baby-mother compared too hands-on approaches that exist today.
The future of artificial womb technology could be truly revolutionary for premature infants or those who can’t carry due to medical reasons. But it raises important questions about the ethics surrounding surrogacy and reproductive technologies.
Despite any impending debates, we must commend these researchers on their innovative work that may change lives in a way no one imagined possible!
Frequently Asked Questions About Artificial Womb Technology
Artificial womb technology may be a complicated and futuristic concept, but it is generating interest among scientists as well as the general public. Some people are curious about how it works or its purpose, while others worry that it could replace traditional pregnancy. In this piece, we will answer some of the most commonly asked questions about artificial womb technology.
What is an artificial womb?
An artificial womb- also known as ectogenesis- is a device used to help grow embryos outside of the human body by providing all necessary nutrients and conditions so they can develop into healthy fetuses.
Who came up with the idea for an artificial womb?
The concept of an artificial womb was first introduced in science fiction novels and movies. The scientific process began in the 1950s when researchers started experimenting with growing fetuses outside of their mother’s bodies using animal models like sheep.
Why do we need an artificial womb?
Artificial wombs have extensive potential however two chief benefits that experts often cited raising preemies without fear, neonatal research to study early development and abnormalities more closely than current methods allow
How does an artificial womb work?
An artificially created environment similar to a natural uterus in terms of temperature ,pressure,salt levels,minerals etc provides everything necessary for growth typically via amniotic fluid-like substance which contains all necessary nutrients for fetal development along wioth oxygen through blood circulation provided .A membrane-based system consisting prevents fetus from obstruction whilst preventing bacteria from infiltrating housing too.
Could an Artificial Womb completely replace Pregnancy?
While further testing would certainly be needed before any widespread introduction of ARTIFICIAL wombs occur arguably initially only those having difficult pregnancies or high-risk births might succumb beenfitting greatly,Lots has yet unknown if full replacement possible without physical emotional contact during gestation replacing multiple aspects integral beyond biology alone making under standard circumstances :
Is there evidence proving that these machines are safe for babies ?
Although prototypes still being tested initial results proved to be fairly promising, with all visible signs of healthy growth and development initially observed. However, more tests will need to be conducted on larger scale along different developmental stages to fully verify long-term safety
What are the ethical issues surrounding artificial wombs?
The idea has been criticized by some groups calling it “unnatural”, especially concerning any potential negative effects for women .Moreover , questions over use practices outside of necessary medical cases argue moral standards questionable particularly when connected financial motives leading exploitation or devaluing motherhood important human experience.
In conclusion then :
Artificial womb technology raises hopes for improving neonatal care research alongside lessening risks associated with pregnancies even in difficult circumstances,but its introduction looks set only come gradually perhaps targeting particularly high-risk births rather than replacing traditional methods just yet.Whilst there remain legitimate concerns as highlighted above about appropriate usage standards ethics etc generally speaking Artificial Womb definitely provides a new ray of hope around fetal health well-being optimism whereby additional studies efforts towards improvement ought carry on regardless!
The Top 5 Facts You Need to Know About Artificial Womb Technology
The idea of growing a baby outside the human body might sound like science fiction, but with recent advancements in medical technology, artificial womb technology is no longer just a plot point in movies. Today, doctors and scientists are working on developing this futuristic concept to prevent premature births and give babies born too early a better chance at survival.
Here are the top 5 facts you need to know about artificial womb technology:
1) What Exactly Is an Artificial Womb?
An artificial womb or external uterine environment (EUE) is a device that mimics the conditions inside a mother’s uterus that allow fetal development during pregnancy. Made out of materials such as silicone or plastic, it provides nourishment and oxygen while keeping harmful substances away from the fetus.
2) How Does It Work?
Depending on the model, an EUE can vary in design and function, but most operate by using amniotic fluid replacement therapy (AFRT). This process involves inserting a tiny tube into the umbilical cord and pumping special fluids containing nutrients through it to support life.
3) Why Are We Developing Artificial Wombs?
Premature birth rates continue to rise globally year after year with devastating effects for families who experience them. The use of an EUE could provide significant benefits for babies born too early or those with complications requiring extended hospital stays such as preterm labor, uterine abnormalities, preeclampsia among other factors making their chances slim if kept within traditional incubators.
4) When Will They Be Available?
While researchers have made significant progress towards creating stable devices capable of supporting human fetuses prematurely born around 22-23 weeks street gestation; artificially-grown infants remain years if not decades away from clinical reality. With many trials still ongoing today due do potential long-term side-effects – ethical considerations regarding their creation arise constantly – there remains much work before we see these technologies coming ever close toward full public distribution.
5) Is This Technological Advancement a Good Thing?
Artificial womb technology could be an innovative solution towards improving healthcare for our most vulnerable infants – research is ongoing and the benefits to infirm newborns are endless. However, concerns *do* arise about its sterilization process, risks associated with constant maintenance infections being top of mind: But given enough time and resources dedicated into trials – it may prove useful in successfully overcoming some of life‘s toughest complications that occur during childbirth.
Finally,
Artificial womb technology has been a subject of interest around the world since early 2002; now in 2021, we have seen significant progression toward creating these advanced incubator systems capable of assisting premature babies throughout critical phases within clinical care. Otherwise long drawn hospital stays or worse circumstances affecting their survival chances over longer gestational periods priorly considered incurable conditions posing much deeper ethical considerations years ago when such thought experiments were more hypothetical than real science — transforming this realm options–inducing hope for parents’ everywhere facing difficult pregnancy situations today.
Exploring the Potential Benefits of Artificial Womb Technology
Artificial womb technology, also known as ectogenesis, has been a topic of discussion in the scientific community for decades. It involves creating an environment outside of the human body to help fetuses grow and develop until they are ready to be born. While this may seem like something out of science fiction, it is actually becoming more feasible with advances in medical technology.
The potential benefits of artificial wombs are numerous and far-reaching. Here are just a few:
1) Reduced Risk of Complications
Pregnancy can come with many risks such as pre-eclampsia, gestational diabetes, hypertension, and even maternal mortality. An artificial womb could potentially eliminate these risks by providing a controlled environment where fetal growth can be monitored and regulated without impacting the mother’s health.
2) Increased Neonatal Survival Rates
Preterm birth is one leading cause of infant mortality worldwide. Artificial wombs give us hope that babies born too soon can survive earlier and better than they ever had before. In fact, researchers have already successfully grown lamb fetuses in artificial wombs for up to 28 days.
3) Opportunities for Genetic Modification
Artificial womb technology opens up avenues for genetic modification research beyond what would be possible through traditional reproduction methods alone. This offers new possibilities for preventing certain genetic disorders or treating diseases within utero.
4) Greater Autonomy For Women
This point sounds surprising if you consider women undergoing pregnancy which requires utmost care throughout but hear me out here – Reproductive autonomy refers to decision-making control over one’s reproductive processes including matters involving contraception use; prenatal diagnostic testing; continued pregnancy; abortion access among others based on personal beliefs & circumstances surrounding their lifestyle choices- Artificial Womb technology has the ability grant that choice during child-bearing process as per woman’s convenience , ultimately supporting gender equity progress.
5) Alleviation Of Social Stigma
Lastly,stigmatization associated with unplanned pregnancies rarely affects men perception towards dating , marriage or casual sexual encounters . ART enables fetus to be removed from mother’s womb which could alleviate societal stigmatization associated with unplanned pregnancies. This technology not only keeps fetuses safe but also affords the opportunity for mothers to make a knowledgeable choice about their pregnancy while avoiding unwanted judgments.
Artificial Womb Technology is still in its infancy, both literally and figuratively, however; it has endless potential benefits compelling enough to continue developing the research around how we can optimize fetal growth through ectogenesis outside of human body.Although this may seem like a panacea-like solution,it must undergo rigorous medical testing with valid clinical trials prior being released into mainstream usage under regulatory agencies supervision. Even so, exploring further investigation into artificial womb technology highlights opportunities for increased control & personal decision-making during pregnancy along with providing means for saving life of countless pre-mature newborns ultimately signifies progress towards equitable prenatal care that encompasses all women – regardless of their background!
The Ethical Debate Surrounding Artificial Wombs and Reproductive Rights
The possibility of artificial wombs has been the subject of scientific curiosity for many years. The concept seems both fascinating and terrifying – a machine that can grow human beings instead of a mother’s body? It certainly sounds like something out of science fiction, but it is actually quite real.
The technology to create an “artificial womb” already exists in experimental stages. Essentially, this involves creating an environment that mimics the conditions inside a uterus in order to grow an embryo into a fully-formed baby without intervention from a biological mother. In some instances, these developments could be life-saving for premature babies who are born too early and require extended care.
However, as with many new advancements in medical technologies, ethical questions arise around what rights should be afforded to those involved in such processes. For example: believing children growing up independent from their mother might result in implications on emotional bonding later on.
One major concern is whether or not women will become obsolete altogether when it comes to reproduction; further fueled by older discussions about societal trends moving away from heteronormativity and more developmental advancements being submitted towards egg freezing and adoption practices over pregnancy involving female bodies entirely. This fear would likely spark arguments differing based off individual moral beliefs regarding gender equity versus procreation ethics.
Another argument against artificial wombs tackles inequality – specifically between rich communities having better access compared to poorer ones relying solely upon traditional methods outside of laboratory-created procedures such as surrogacy etc.. Would only the wealthy benefitting have unique individuals grown due to advanced technological growth whilst others still continue struggling?
On the other hand there are people believe this technology has potential for liberating individuals looking to reproduce without any restrictions based off external factors which they may normally face under current laws (e.g., ageism).
They also believe that it could help alleviate practical concerns related with IVF treatments today by eliminating instances where healthy embryos fail transplantations leading recipients requiring subsequent additional costly approaches following failed pregnancies or other medical conditions preventing successful motherhood.
Overall, the ethical debate surrounding artificial wombs is a complex one that requires much consideration before societal implementation. The science may be there, but as with all major shifts in technology or medicine, we must ask ourselves what laws and regulations can help maintain balanced accessibility whilst minimizing additional inequalities and avoid any negative consequences of developing such advancements moving forward
Overcoming the Challenges of Developing and Implementing Artificial Womb Technology
The idea of an artificial womb is one that has been floating around for a while now, and it’s not hard to see why. Developing such technology would have the power to revolutionize reproductive science as we know it, opening up a world of possibilities for families struggling with infertility or preterm labor complications.
But as exciting as this concept may be, developing and implementing an artificial womb also comes with its fair share of challenges. From ethical considerations to technological hurdles, there are numerous obstacles standing in the way of bringing this futuristic-sounding technology into reality.
One major challenge facing researchers attempting to develop the first functional artificial womb is simply understanding all of the complex biological processes involved in fetal development. A real-life uterus orchestrates a wide range of interconnected physiological events, including hormone production and regulation, nutrient transport, respiration and waste elimination – among others. All these factors must be precisely replicated by any form of artifical wombs during pregnancy for successful gestation outside a mother’s body which requires extensive research on embryonic development biology.
Another significant obstacle facing those striving towards building an effective model lies at the ethical boundaries within medical practices especially since moral philosophies like consequentialism vs deontological ethics doesn’t give clear answers over what technologies should or shouldn’t be allowed if they’re feasible enough. The safety issues surrounding genetic modifications & DNA reprogramming could pose serious threats even though new design approaches are being deeply considered presently – making sure their practices will meet certain minimum regulatory measures can go a long way!
Of course, beyond these scientific and practical barriers lie many more socio-cultural implications too that need careful consideration prior to launching any radically innovative approach in mainstream society accross varying cultures around the globe.The notion that pregnancy could occur entirely outwith traditional ‘natural’ methods might raise some concerns about whether important societal values centered around parenting & family-building alters when removed from biological reproduction norms ultimately leading to either embracement or rejection based on societal beliefs.
But while it may seem like the challenges facing artificial womb development and implementation are insurmountable, many experts in this field remain hopeful &to some degree suggests that the benefits of successfully building such technology outweigh their risks. The ability to give premature babies a better shot at life, for example, or help infertile couples conceive would mark an unprecedented leap forward as advancements taking us closer towards Artificial General Intelligence already begin revolutionising almost every sector imaginable including health care provision hence representing an unparalleled next level breakthrough given its potential capabilities.
In summary maybe not today or tomorrow but with continuing research and technological developments,the prospect of creating a fully functional gestating system outside traditional pregnancy methods by way of artificial wombs can’t be ruled out just yet!
Table with useful data:
| Date | Event | Significance |
|---|---|---|
| 1950s | Development of artificial placenta | Possible solution for premature births and low birth weight babies |
| 1996 | First successful pregnancy using artificial womb in sheep | Opening doors for human development |
| 2017 | Harvard University’s successful cultivation of 50 premature lambs in a device called BioBag | Further research and advancements toward the possibility of artificial womb technology for human births |
| 2021 | Creation of an artificial placenta on a chip by University of Michigan | Promising potential for individualized medical treatments, including disease modeling and drug testing |
Information from an expert
As someone who has closely studied artificial womb technology, I believe it has the potential to revolutionize how we approach pregnancy and childbirth. With this technology, we could help babies who are born prematurely or with health issues develop in a safer environment than current neonatal intensive care units can provide. Additionally, it gives women who may not be able to carry a child themselves due to medical conditions the ability to have biological children without relying on surrogacy or adoption. While there are still many ethical and legal questions surrounding the use of artificial wombs, their possibility for improving reproductive healthcare is certainly worth exploring further.
Historical fact:
Artificial womb technology was first introduced in the 1950s by Dr. John C. Beck and colleagues at the University of Pennsylvania who successfully grew premature lambs to term using an artificial uterus filled with amniotic fluid.

![Unlocking the Power of Social Media Technology: A Story of Success [With Data-Backed Tips for Your Business]](https://thecrazythinkers.com/wp-content/uploads/2023/05/tamlier_unsplash_Unlocking-the-Power-of-Social-Media-Technology-3A-A-Story-of-Success--5BWith-Data-Backed-Tips-for-Your-Business-5D_1683142110-768x353.webp)
![Revolutionizing Business in the 1970s: How Technology Transformed the Corporate Landscape [Expert Insights and Stats]](https://thecrazythinkers.com/wp-content/uploads/2023/05/tamlier_unsplash_Revolutionizing-Business-in-the-1970s-3A-How-Technology-Transformed-the-Corporate-Landscape--5BExpert-Insights-and-Stats-5D_1683142112-768x353.webp)
![Discover the Top 10 Most Important Technology Inventions [with Surprising Stories and Practical Solutions]](https://thecrazythinkers.com/wp-content/uploads/2023/05/tamlier_unsplash_Discover-the-Top-10-Most-Important-Technology-Inventions--5Bwith-Surprising-Stories-and-Practical-Solutions-5D_1683142113-768x353.webp)